My gallbladder story is quite short really and uncomplicated in comparison to others. I’d never really experienced any problems with my gallbladder. Although, looking back, there was a time I had a sharp and horrendous pain in my upper-right abdomen in 2012 one day while at work. The pain was severe and my boss called an ambulance which came right away and injected me with a load of pain killers and muscle relaxants. I went home and slept it off and the pain was gone within a few hours so I never even went to a doctor about it. Maybe, that was an attack, maybe not.
Fast-forward to the beginning of February 2019. I was still being investigated after a complicated case of diverticulitis that resulted in the perforation of my bowel and a battle with sepsis. My constant lower-abdominal discomfort caused my gastroenterologist to send me for a full abdominal ultrasound. He wanted to rule out abscesses, cysts and adhesions so requested a scan of the whole abdomen.

At the ultrasound, the doctor started snapping pictures of my organs and measuring dimensions, then, the moment he got a clear image of my gallbladder, he asked ‘Are you on the waiting list to get this removed?’, ‘No’ I replied, ‘Why do you ask?’ and he told me that there were a few small stones in there, but more importantly a polyp. I told him I had no idea and hadn’t had any symptoms of things not working well. Anyway, at the end of the ultrasound, he gave me all the printed photographs and a written report detailing what he had found and told me to go back to my gastroenterologist as soon as possible.
The gastroenterologist told me that it would need to be removed and set up a meeting with a surgeon for a few days later. He looked at my results, agreed that it needed to be removed because of the potential for the polyp because of its size to be a risk. He penciled me in for two weeks later to get it removed. In the mean time, he told me to eat a low fat diet and gave me a list of foods to avoid. (I’ll post about this soon, I promise)
Before I knew it, it was removal day. At 7:30am I hopped onto the trolley and was taken down to surgery. I watched the staff running around doing last-minute checks and preparation. It was fun chatting to the hospital porter who spoke pretty good English and was so smiley. I wasn’t particularly nervous or scared, I deal with hospital and needles etc pretty well and I’m not someone to get themselves into a state about a surgery. I’m sure I was mid-sentence joking with the surgeon and porter as I drifted off into a deep sleep and the surgery began.
In what seems like no time at all, I wake up in a different room with an IV in the opposite arm and a drain coming out of a hole in my upper-right abdomen. I look to my right and the porter is stood there smiling. I smile back and say ‘I need to sit up’, He immediately props the trolley up and hands me a little sick bowl….no, I say, I feel like I can’t breathe. So, he calls over a nurse who measures my oxygen levels and rushes off and comes back with a mask. I’m hooked up to oxygen and starting to catch my breath. Five or ten minutes later, the porter takes me back to the ward where my boyfriend was waiting to see me. He seemed worried, I asked him what the problem was and it was only then, that he told me that the surgery was expected to last maybe an hour and a half, but that I had been there for over four hours due to it being a tricky surgery. I hadn’t even noticed what the time was.
I expected to be in major pain the rest of the day, but other than a horrible discomfort in my back and shoulders, I had no pain at all. I refused dinner when the nurse brought it. I wasn’t hungry at all and the noodle soup did NOT look appetizing at all. I was alone now because my boyfriend had left for work. I forgot I had the drain and as I got up out of bed and went to the bathroom, I must have moved the drain a little and it was a bit sore. After the effort of that, I went back to bed and was in a little pain. The nurse came to check on me and when I told her it was sore, she injected something into my IV and the pain subsided and I drifted off again.
I woke up the next morning feeling quite chipper. I still had some discomfort in my back and chest from the gas, but was keen to get up and about. I got up had a wash, brushed my teeth and did my hair. Then I got changed. When the nurse offered pain relief via the IV, I declined since I didn’t have any pain except for the gas pains. I got up and walked around the ward and the catering team brought me a chamomile tea which I sipped at.
My surgeon came in to speak to me and told me not to lift heavy things or to strain when going to the bathroom due to the risk of getting a hernia. I was a little worried since I had pushed a bit going to the toilet in the morning, but it was okay, the stitches had held. He removed the drain and replaced my dressings. Before telling me to take almost 3 weeks off work and discharging me from the hospital. He told me to clean my wounds and replace the dressings each day. He also advised me to take a paracetamol if I was uncomfortable, but to contact him if I had severe pain, or jaundice.
I didn’t even need the paracetamol. Recovery wasn’t too difficult, but I stuck to the post-op gallbladder diet that he gave me. (I promise I’ll write about this, too) The one thing I had a problem with, was laying down. The stitches were tight and I couldn’t lay down or get up, so for the first week, I slept sitting up on the couch. It wasn’t a problem.
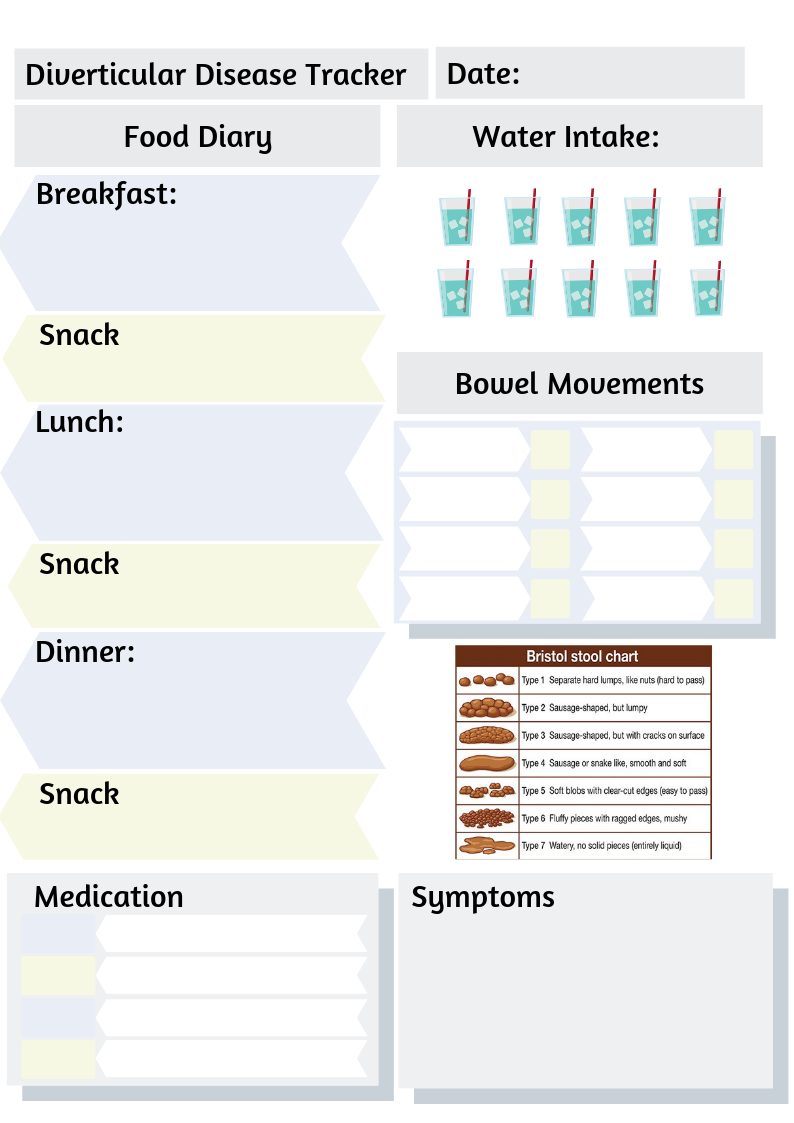
I used glycerine suppositories everyday to keep me going to the bathroom without effort. As the days passed, I found doing things even easier and as time passed I found myself able to tolerate more foods. The surgeon checked up on me regularly via telephone and asked me to send him pictures of the healing incisions on Viber. They were all doing great accept for my belly button which was weeping and a little sore and hot to the touch. Although, the surgical incision in my belly button did become a little infected and I had to pack it and take antibiotics, but within a week, it was much better and I could go to have the stitches removed. I had to be careful to stay near a toilet after trying a new food though because a few times in those first couple of months, I experienced dumping syndrome and had to make a bee line for the bathroom.
Post-op, life isn’t much different for me. I sometimes still get dumping syndrome, particularly if I eat something too fatty. Otherwise, I don’t have any real symptoms…just like before my op. However, it’s nice to know that the polyp was removed and won’t be causing any trouble in the future.
So, if you’re having your gallbladder removed. Don’t worry. It isn’t as bad as you might think. If you are suffering with a lot of anxiety, tell your doctor. There are things they can do to help you relax and to reassure you about the surgery. Of course, everyone’s gallbladder story is a little different. But, this is mine and from my experience, I feel it wasn’t a bad or scary experience. But, it is so important to take time out to recover.
My advice is to not push yourself or overdo it during your recovery – you may regret it. Also, don’t expect to feel back to normal immediately. The human body is amazing, but it certainly needs to be given the time to heal after surgery.