
Wishing you all the best this Christmas and New Year!
May your 2020 be full of love, health and happiness.
Useful information for any digestive ailment!


Wishing you all the best this Christmas and New Year!
May your 2020 be full of love, health and happiness.

When diagnosing diverticulitis, the first thing that doctors usually do is carry out a blood test followed by other tests such as CT scans, X-rays and even ultrasounds.

Full Blood Count
The full blood count can tell doctors a lot about your current health. The number of red blood cells can tell doctors if you’re anaemic and perhaps losing blood. But one of the most important markers in a blood test when trying to check for diverticulitis is the white blood cell count.
White blood cells are a part of the immune system and are responsible for fighting diseases and illnesses. When a pathogen (harmful bacteria or virus) enters the body, it is identified by the immune system which then increases the number of white blood cells. An amount of white blood cells higher than the normal range could be considered to be a sign of infection. However, it is possible to have diverticulitis but not have a measurable increase in white blood cells. So a normal blood result doesn’t necessarily mean that you don’t have an infection or inflammation in the bowel.
CRP (C-Reative Protein)
CRP is known as an inflammation marker – it is a protein released by human tissues when they are inflamed. The higher the amount of CRP in the blood, the more inflammation there is. Having elevated CRP in addition to abdominal pain and other symptoms is a good indicator of diverticulitis. However, your doctor should also check carry out an abdominal examination too just in case the inflammation is coming from somewhere else.

Abdominal Examination
It’s likely your doctor may carry our an abdominal examination. This is where the doctor will press on your abdomen to discover where the pain originates and if it is the bowel that is inflamed. It’s important to be very honest about the pain you are feeling at this point so that the doctor can rules out any other issues or sources of inflammation.
CT scan
This is usually the most effective way to diagnose diverticulitis. A CT scan can be done with or without contrast, but contrast certainly helps when interpreting the results. The two main types of contrast are oral and intravenous (IV). The oral contrast is often a liquid mixed with water that you drink before the scan. It helps to highlight the digestive tract on your scan. The IV contrast is injected into a vein and reaches the tissues and helps them show up better on the scan. Some hospitals may choose to have their patients take both types of contrast. However, it is important than you let the doctor know of any allergies you have before you receive any contrast agents.
A CT scan is painless and just requires the patient to hold their breath for short periods. Let the technician or doctor performing the scan know if you suffer from asthma or COPD or any problem that makes you find it difficult to hold your breath.
After the scan, your results will not be ready immediately since they will need to be looked at by a doctor and a thorough report written. See my post on CT scans for more information.
X-rays
Some doctors may choose to send their patients for X-rays. This is to check for perforations in the bowel since X-rays can easily pick up excess gas in the abdomen that may be leaking out from the bowel. The results of an X-ray are much more immediate which is why this test might be chosen particularly if the patient is in a lot of pain or has a history of perforations and sepsis.
Ultrasound
Again, some doctors may want to send their patients for an ultrasound. This is very common during first time diagnoses when patients are doctors don’t know that the patient even has diverticular disease yet. An ultrasound may also show an abscess or cyst as a result of diverticulitis. It may also be able to detect excess air of material in the abdomen. However, it is not as clear as a CT scan, but the results are more immediate.

Why don’t doctors use colonoscopies to diagnose diverticulitis?
It’s very rare that a doctor would use a colonoscopy to diagnose diverticulitis because while a patient has an infection, it would be very painful and a little dangerous to insert an endoscope. There is a chance that the colonoscopy during an infection could make it even worse or could even cause damage to the colon.
Have you been diagnosed with diverticulitis? Which methods did the doctors use to diagnose you?

So, you’re waiting to get your gallbladder removed – Don’t worry, it’s not as bad as it sounds. In fact you can read about what gallbladder removal surgery entails here or you can read my own story on getting my gallbladder removed.
To avoid extremely painful gallbladder attacks or the worsening of your condition while waiting for your surgery, you can aim to have a low-fat diet. A diet low in fat will hopefully ward off any painful attacks and prevent gallstones from getting larger.
You can eat:
Avoid:
Try not to do a no-fat diet because this can cause the gallbladder to become even worse. Stick to low-fat and try not to eat large portions. Instead aim to have smaller snacks and portions throughout the day. This will help your gallbladder keep working and prevent discomfort after eating.
Want to know more about what comes next? Read Gallbladder Removal Surgery – Cholescystectomy and let me know what you think.

Gallbladder removal or a cholescystectomy is a common surgery carried out by surgeons all over the world. The gallbladder is an organ located in our upper-right abdomen, just beneath the liver. It is the place where bile is stored. Bile is a yellow/green liquid produced by the liver when it breaks down substances in the body (including our old red blood cells).

The job of bile in the body is to emulsify fats – it does this by breaking up the fats and oils we consume into smaller droplets so that our body can digest it more easily. It also helps to neutralise the acidic chyme (food + stomach acid mixture) that leaves the stomach and enters the small intestine.
The reasons for a cholescystectomy include;
So what is the surgery like?
Well, these days, most cases are done laparoscopically. This means that it is done using several small incisions in the abdomen (for example in the navel, right side of the abdomen and possibly an incision in the centre of the upper-abdomen. Most patients have three or four incisions, but there are cases of people having less or more. The surgery is carried out under general anaesthetic. This means that you’ll be asleep and unaware of anything going on. Most patients are intubated (with a breathing tube) for this procedure, but are not usually catheterised. The surgery usually lasts between one and two hours. Depending on your hospital, some people may go home the same day and in others, they may be asked to stay in hospital overnight.
If you have an open surgery, the surgeon will make a large incision in the upper-right abdomen and take the gallbladder out from here. This is avoided where possible since it increases the length of time needed for recovery and hospitalisation.
During a laparascopic surgery, the surgeon will inflate the abdomen with gas. This helps provide more space in side to move around and perform the procedure. Then a camera will be inserted into one of the incisions so that the surgeon can see what he is doing. After this, various tools will be inserted into incisions to cut the gallbladder free. Medical titanium surgical clips will be placed to cut off tubes that connected the liver to the gallbladder. These metal clips will remain inside your body for the rest of your life.

Of course like any surgery, it does carry risks and there are complications that can arise. However, for this surgery, complications are rare and most patients deal with it very well.
What is the recovery period like?
Well, for me, it wasn’t too difficult. But everyone heals at different speeds and has a different experience without their gallbladder. Some people are back at work within a few days, and others may take a couple of months to get back to normal.
My advice is not to rush yourself. Recovery is an important process for our body and to recover well you need to rest and relax while trying to stay healthy. Your surgeon will give you some guidelines for aftercare and recovery, so it’s important to stick to those as much as your possibly can.

General guidelines include:
To read about my gallbladder story click here! Want to share your story? Get in touch with me so that we can tell your story, too!

People who have digestive conditions often find that their symptoms differ from day-to-day. Some days, they might feel okay and at other times, they may experience a ‘flare up’ of their condition. This happens with lots of digestive ailments such as IBS, diverticular disease, Crohn’s and other IBDs.
During these flare ups, lots of patients are advised to eat a low-residue diet. But what exactly is that? Well, it’s a diet that produces little waste in the bowel and can be mostly absorbed by the body. The foods that are low-residue tend to be low in fibre (US: fiber) since fibre cannot be absorbed by the body and so makes up the bulk of our stools.
Eating a low-residue diet allows our bowel to rest a little until we are feeling better. But, don’t worry, it’s not as restrictive as you might think. In fact, it’s definitely possible to enjoy your food while on a low-residue diet.

So, what foods are included in a low-residue diet?
Go ahead :
In moderation:
Avoid:
NOTE: A low residue diet is NOT a low FODMAP diet. These are different things. Some people get confused between the two. For now, I haven’t written a post on a FODMAPs, but when I do, I’ll link it right here.
Of course, as with any food guidelines, you may find that some of the foods on the ‘go ahead’ or ‘in moderation’ lists bother you and cause undesirable symptoms, if this happens, just simply cut it out of your diet.

Having trouble figuring out which foods are causing you issues? Use my Diverticular Disease Tracker to monitor your food intake and any symptoms you get (You don’t need to have diverticular disease to find this document useful). You may also need to introduce new foods gradually and one at a time. Also, when you are over your flare up, it’s important to slowly increase your fibre intake otherwise you may cause yourself discomfort.

This article is for people suffering with an episode of Diverticulitis rather than just having Diverticular disease/Diverticulosis.
Not sure what the difference is? Then check out my post about Diverticular Disease/Diverticulosis Vs Diverticulitis.
Diverticulitis is an inflammation or infection of one or more diverticula (pouches) in the bowel. It can cause diarrhoea, constipation, nausea, loss of appetite, abdominal pain or discomfort, blood in the stools, a fever and various other symptoms. If you have been diagnosed with diverticulitis, chances are that you’ll be taking antibiotics to help clear the infection. You may also be advised in some cases to undertake a clear liquid diet. For a detailed explanation of what this entails, click here.
You may also be told you are allowed a soft foods/low residue/low fibre diet. This means plain/bland and easily digestible foods that do not contain much fibre. This allows the bowel to rest.
Include:

Please avoid:

Remember that everyone is different and sometimes even these foods may cause discomfort. Because of this, I recommend tracking your food and water intake alongside your symptoms to have a clear picture of what is going on. You can do this by using my Diverticular Disease Tracker which is available to download for free and print out immediately.
In addition, I’d recommend eating slowly, and having small portions regularly so that your digestive system isn’t overwhelmed by large meals. You can pick up more tips for good digestion by reading this post.
What do you eat when you have diverticulitis? Are you able to tolerate all of the foods on this suggested list? If not, which are unsuitable foods for you?

This article is for people wanting to know about foods to eat if they have diverticular disease/diverticulosis NOT diverticulitis. If you aren’t sure what the difference is or what you have, click here to find out.
One of the most common questions people have when they are diagnosed with Diverticular disease (DD) /Diverticulosis is ‘What can I eat?’. Unfortunately, there is no clear answer to this question. As an active member of various Facebook support groups, I see people all the time asking can I eat this or that. And the answer to the question is as follows.

There is no answer. Based on the latest medical research, there are no disallowed foods for diverticular disease/diverticulosis. This means, anything you ate before diagnosis, should be safe afterwards. Since you ate them just fine before you discovered the diverticula/pouches in the bowel. However, it is largely believed that eating a diet high in fibre is beneficial for those who have diverticular disease since it keeps the bowels moving and prevents stool causing the diverticula to become inflamed or infected. So perhaps upon discovering you have diverticular disease, you may choose to adopt a higher-fibre diet or a healthier one. This could include swapping white bread, rice and pasta for their healthier brown alternatives, eating more fresh fruit and veg or perhaps eating a high-fibre cereal for breakfast. However, there are cases where a high-fibre diet doesnt work out for various reasons and so, you may be advised to adopt a low-fibre diet instead.

Some doctors will advise their patients that they shouldn’t eat seeds, nuts, popcorn, sweetcorn, etc due to the chance of them being lodged in the diverticula/pouches. Although, current research shows this not to be the case. However, some people do have problems with these foods and if it makes you feel better to avoid them, then that’s fine, too.
A lot of discovering what you can eat, is about trial and error. Everyone is different. Many people with diverticular disease/diverticulosis also suffer with other digestive problems such as IBS that can cause symptoms in response to particular foods. So my advice is that if you are feeling unwell, you can try an elimination diet, or you can simply go day by day and keep track of your food intake by keeping a food diary. I’d recommend for those newly diagnosed especially, keeping track of your food and water intake, your symptoms and your bowel movements. You can do this easily using the Diverticular Disease/Diverticulosis Tracker which you can find here and download for free. It includes instructions for how to fill it out. You can even take your completed tracker pages to the doctor or nutritionist so that they can help you look at what foods may or may not work well with you and your needs.

Some advice I can give to ALL sufferers of Diverticular Disease/Divertiulosis is to drink LOTS of water. Two to three litres (4 – 6 pints/70-100 fl. oz) per day. This will help keep you hydrated, healthy and prevent constipation. Also chew your food well and avoid large portions. In fact, simply following my Tips for Good Digestion may help you avoid digestive discomfort.

If you’ve got diverticular disease (DD)/Diverticulosis, you may be unlucky enough to experience diverticulitis. Don’t know the difference? Check out my post on Diverticular Disease/Diverticulosis Vs Diverticulitis. Diverticulitis is an inflammation or infection of one or more of the diverticula (pouches) in your bowel. Diverticulitis can vary in severity and can go from being a mild flare up, to an infection so severe that it can carry life-threatening complications. So, what can you do if you suspect you may be getting a flare up?
For a start, symptoms of a flare up can include:
If you are experiencing some of the symptoms above, it’s a good idea to prepare for a flare up by doing the following things:
DO:
If you suspect you may be experiencing a flare up, there are a few things you should avoid doing in order to not make things worse.
DON’T:
These tips and tricks may be able to help you rest the bowel before medical treatment is required. However, if your symptoms become worse or do not subside, it’s important to seek advice from a medical professional.
If it turns out antibiotics are required, there are a number of things you could be prescribed. For example, common antibiotics include: Ciproxin, Flagyl (metro), Co-amoxiclav, Augmentin and several others. However, Ciproxin and Flagyl are the ones most suitable for those with a penicillin allergy. Please note that some of these antibiotics have some significant side-effects and you should make yourself aware of these by reading the leaflet or discussing it with your doctor before you take them.

In a more severe situation, you may even be admitted to hospital to receive treatment for diverticulitis. Here, they will usually give you antibiotics, fluids and pain relief intravenously. You can read about what I like to pack in my hospital bag here.
What symptoms do you experience before a flare up? Have you managed to treat a flare up without antibiotics? How did you do it?
Support the author and buy her a coffee by making a donation here: paypal.me/haylaki

Is there a difference between diverticular disease/ diverticulosis and diverticulitis?
Yes, quite an important one, too and here’s what it is…
DIVERTICULAR DISEASE/DIVERTICULOSIS
The condition of having diverticula or ‘pouches’ along the wall of the large intestine.

This disease is thought by most medical professionals to be symptom-free. However, lots of Diverticular disease (DD)/Diverticulosis sufferers will tell you differently. The truth, really is that it’s not a condition that is very well known and the symptoms of it appear difficult to record and monitor since they vary so much from person to person and can be confused with other digestive tract problems such as IBS.
Generally, it is thought that those who have a diet lacking in fibre or who live an unhealthy lifestyle are more likely to develop diverticula in their bowel over time. However, there are suggestions involving a genetic predisposition to develop them, too.
DIVERTICULITIS
When one or more diverticula becomes infected and/or inflamed.
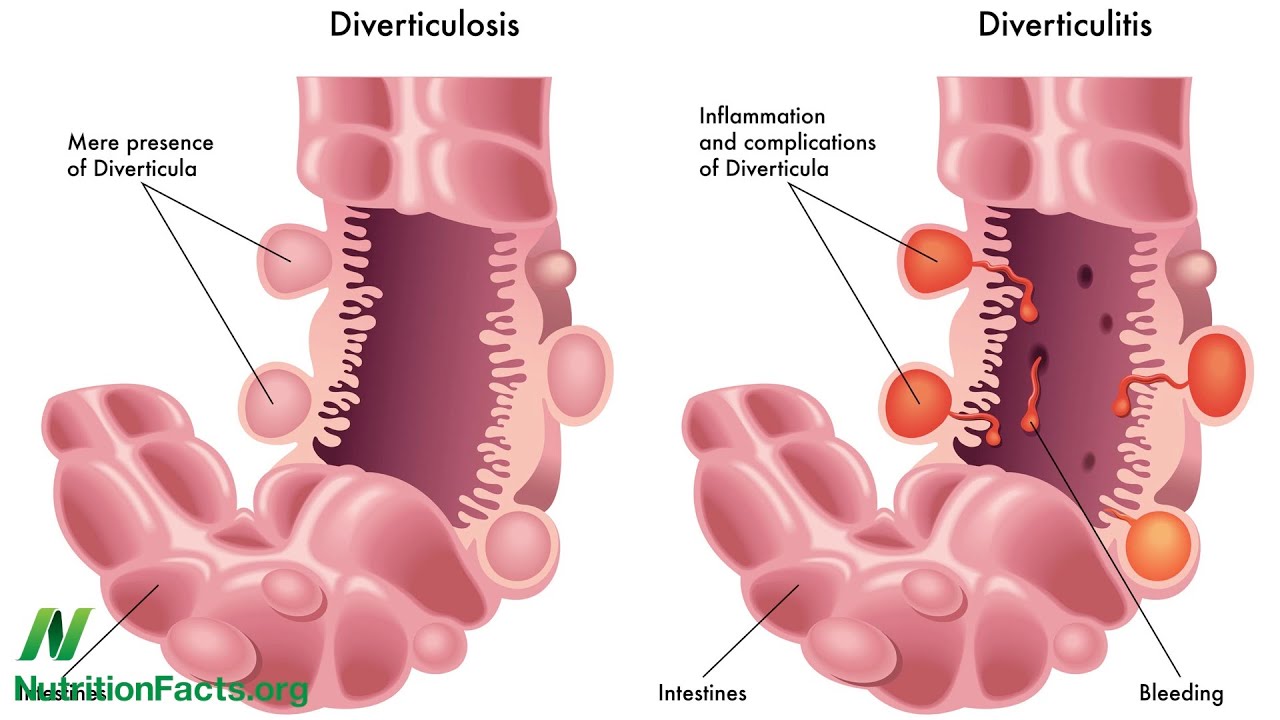
A lot of medical terms or parts of them come from either Greek or latin origins and diverticulitis is an example of this. The –itis suffix comes from greek and means inflammation or infection. We see this with lots of other words too, for example, tonsillitis, arthritis, etc.
Diverticulitis is an infection or inflammation of one or more diverticula in the bowel. The reason for diverticulitis is not well understood, but it is thought that living a healthy lifestyle and keeping stress to a minimum can reduce the likelihood of it taking place. However, there is no guaranteed magical fix-it that will work to keep you free of infection. It is often detected by the use of blood tests and CT scans. However, some doctors use X-rays as a fast way to check for perforations of the bowel, too.
Diverticulitis can vary from being mild to severe with complications. For the very mildest episodes a clear liquid and low residue diet will help you get through. However, for other cases antibiotics may be required or even in some cases hospitalisation and even surgery.
It’s worth mentioning that the overwhelming majority of those with diverticular disease/diverticulosis never get diverticulitis! And, out of those who do get it, only a few get repeated episodes and/or surgery.
So, remember, the diverticular disease/diverticulosis is the presence of diverticula or pouches in the intestine whereas diverticulitis is an infection or inflammation of one or more diverticula. It’s important to know whether a diagnosis of diverticular disease/diverticulosis or diverticulitis is given to know how best to deal with it is.
Do you have Diverticular Disease/Diverticulosis? Have you ever had diverticulitis?

Traveller’s tummy or ‘Holiday tummy’ is something lots of people experience when they go on holiday. Some people get diarrhoea and others find they become constipated or experience nausea. Now, I have blog posts that deal with all three of these issues, but wanted to make a specific post about how to deal with this while on holiday. Whether this is because of the nerves from the flight, new food or water, we can’t be sure. Whatever the cause of your holiday tummy, there are some steps you can take to make sure you’re prepared for every scenario and can kick back and enjoy yourself.

Symptoms of ‘Traveller’s tummy’ can include:
However, if any of these symptoms are severe or do not improve at all within a couple of days, you should seek professional medical advice. You may be able to ask a pharmacist, or speak with a doctor or visit a clinic or hospital if necessary. Remember to take your travel insurance documents and your ID with you when visiting health centres. This will avoid large medical bills.
Drink lots of bottled water
Yes it is more costly and can contribute to plastic waste, but it is definitely the safest bet for something with a sensitive stomach. I opt for bottled water even in regions where I’m assured the tap water is safe to drink. Even just a slight change in mineral content or fluoridation can upset a sensitive stomach and have you heading for the toilet more frequently than you would like. Just be sure to recycle your plastic bottles when you’re done!
Avoiding the local water can be difficult, remember that fruits and salads may be washed in tap water and that the ice cubes used in your drinks may be made from tap water. You can easily ask for drinks with no ice, or if the ice comes from bottled water. You may even wish to use bottled water, to brush your teeth!
Eat sensibly
While I’m sure there are lots of delicious foods to try on your holiday, being cautious while you are experiencing any diarrhoea or stomach problems is a good idea. You can stick to plain foods such as white bread or white rice. Avoid spices and heavily-flavoured foods while your stomach is still unsettled.
After a day or two, your stomach is likely to be a little better and you can be a little more adventurous when sampling the local culinary delights.
Anti-Diarrhoea medication
Anti-diarrhoea medication is very useful to take on holiday with you, but beware, it isn’t recommended for everyone. Those with a stomach bug, food poisoning and diverticular disease/diverticulosis should not take anti-diarrhoea medication unless instructed to by a medical professional. If you’re not sure whether you should be taking it, speak to your doctor or pharmacist before your trip.
Stool softeners
Should you get constipated and find it difficult to eliminate stool, you should try a stool softener. These are often taken in the evening so that they work overnight, meaning by the morning, you are able to have a bowel movement. Common stool softeners include lactulose, milk of magnesia and ;axatives such as Dulcolax or Senna.
However, if you don’t fancy trying medication, up your water and fibre (US: fiber) intake and try get some gentle exercise to get the bowel moving again. You can also eat prunes, figs, Weetabix, licorice and drink prune juice or black coffee. You can also read my post about constipation if you need more information.
Rehydration sachets
As I mentioned in my post about diarrhoea, re-hydration sachets can be extremely helpful when recovering from diarrhoea and re-hydrating your body. During this time, you should definitely avoid alcohol since that can cause further dehydration. This is especially important when visiting a destination with a hotter climate and swimming in the sea.
Have you experienced traveller’s tummy before? How did you deal with it?