A lot of people don’t like to talk toilet, but it’s a natural function of the human body. We all need to eliminate waste from our body and are doing so all the time. For example, we eliminate carbon dioxide by breathing it out, we eliminate broken down proteins and excess water by producing urine, and finally, we eliminate unwanted food and fibre by producing solid faeces (stools/poo/poop).
So, why should we pay attention to the waste we produce?
Because it can tell us a lot about the current state of our health.
There are different characteristics we can look for to judge a healthy bowel movement. Of course, the ideal bowel movement would be easy to pass (without straining or pain) and would be soft but formed and brown in colour. However, for people with stomach problems, we can see a lot of different characteristics so keep reading to find out what your poo could be saying about you.
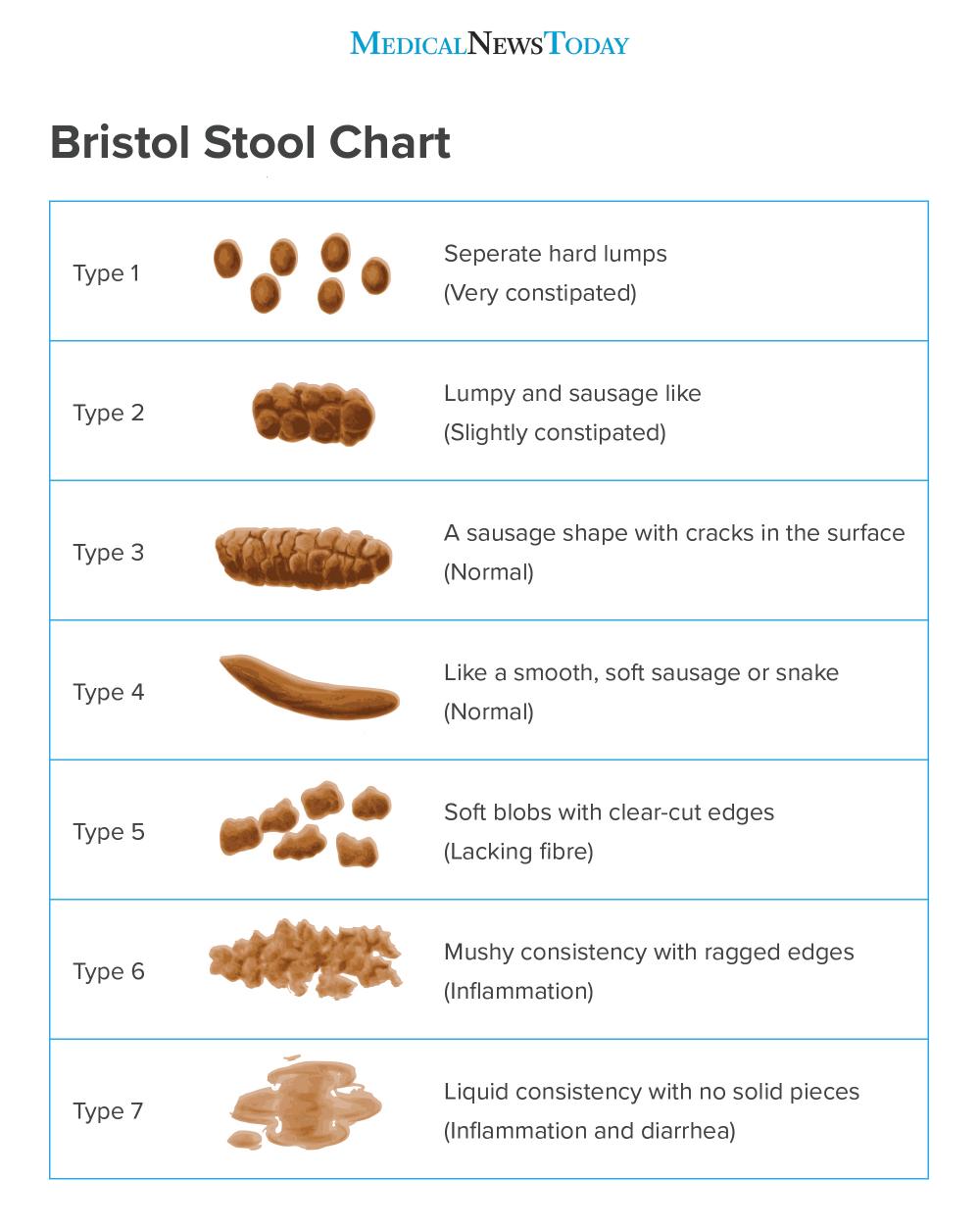
Where does it fit on the Bristol stool chart?
Ideally, you want a Type 4 stool, but a type 3 can happen frequently too.
If you find you are type 1 or 2, you need to read Coping with Constipation. if you have type 5 you may try adding a little extra fibre to your diet, for example with fresh fruit and vegetables or by switching your white bread, rice and pasta with brown alternatives. If however, your stools are type 6 or 7 regularly or over a period of time, you may wish to speak to doctor to figure out what the problem is. If you have type 7, you can look at my post about Dealing with Diarrhoea for tips.
What colour is it?
Stool is most often brown, but sometimes people find that it is other colours. This can be an indication that something isn’t right. So, look below and see if any of the following could be the problem. Please make sure to record any out of character bowel movements and mention it to your doctor.

Are there any of the following?
Now, you’ve looked at the type and the colour. What about anything not mentioned so far?
Undigested food – Sometimes we see pieces of undigested food in our stool. One good example of this is corn. It may appear undigested because it has an outer coating of cellulose. A substance that humans can’t break down easily. Because of this some foods, especially plant-based foods that contain cellulose may appear undigested in our stools. If this happens from time-to-time, it’s no cause for concern. However, if you are finding that a lot of your food is being passed through undigested, it’s worth mentioning to your doctor.
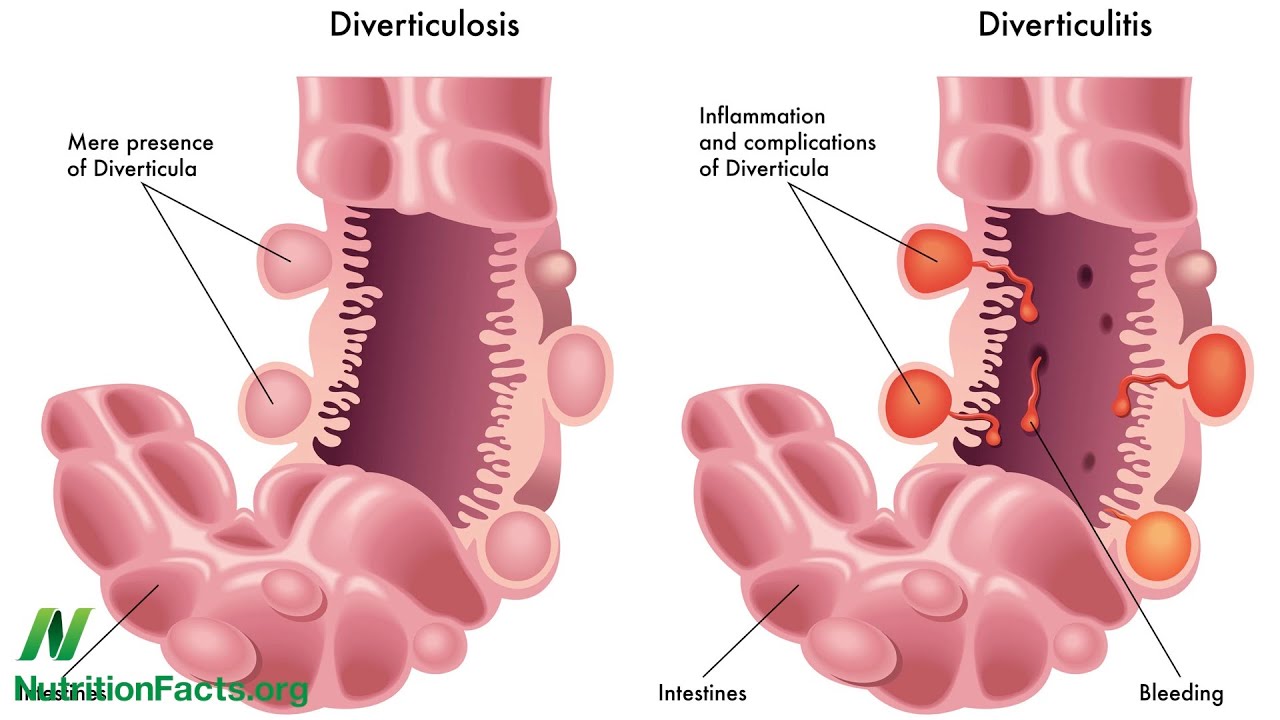
Red blood – seeing a little blood in the stool could be due to various reasons, perhaps haemorrhoids, or a damaged anus. Or it could be bleeding from the lower digestive tract. If this hasn’t happened before, or is a lot of blood or is happening on a regular basis, see a doctor to get checked out.
Mucus – our stool always has mucus in or on it, but often it’s such a small amount that it isn’t visible to us. However, if your bowel movement is accompanied by mucus, it could be a sign of constipation or of inflammation in the bowel. Mucus can vary in colour and appear clear, yellow or even white and can look stringy. Again, if this is happening on a regular basis, it’s important to discuss it with your doctor.
Remember if you have any change in bowel habits, report them to your doctor since they can be a sign of an underlying health issue. Don’t be embarrassed, doctors are trained to discuss bowel habits and reporting yours could change your life or even save your life!