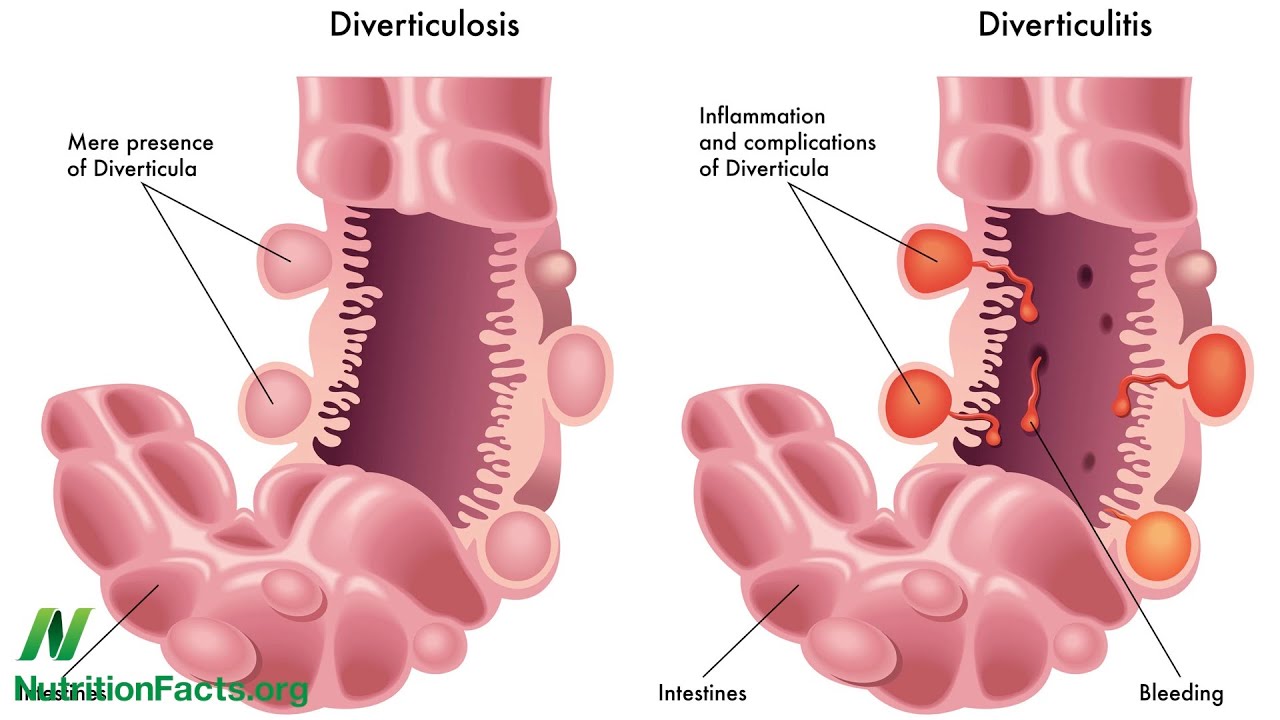
This article is for people wanting to know about foods to eat if they have diverticular disease/diverticulosis NOT diverticulitis. If you aren’t sure what the difference is or what you have, click here to find out.
One of the most common questions people have when they are diagnosed with Diverticular disease (DD) /Diverticulosis is ‘What can I eat?’. Unfortunately, there is no clear answer to this question. As an active member of various Facebook support groups, I see people all the time asking can I eat this or that. And the answer to the question is as follows.

There is no answer. Based on the latest medical research, there are no disallowed foods for diverticular disease/diverticulosis. This means, anything you ate before diagnosis, should be safe afterwards. Since you ate them just fine before you discovered the diverticula/pouches in the bowel. However, it is largely believed that eating a diet high in fibre is beneficial for those who have diverticular disease since it keeps the bowels moving and prevents stool causing the diverticula to become inflamed or infected. So perhaps upon discovering you have diverticular disease, you may choose to adopt a higher-fibre diet or a healthier one. This could include swapping white bread, rice and pasta for their healthier brown alternatives, eating more fresh fruit and veg or perhaps eating a high-fibre cereal for breakfast. However, there are cases where a high-fibre diet doesnt work out for various reasons and so, you may be advised to adopt a low-fibre diet instead.

Some doctors will advise their patients that they shouldn’t eat seeds, nuts, popcorn, sweetcorn, etc due to the chance of them being lodged in the diverticula/pouches. Although, current research shows this not to be the case. However, some people do have problems with these foods and if it makes you feel better to avoid them, then that’s fine, too.
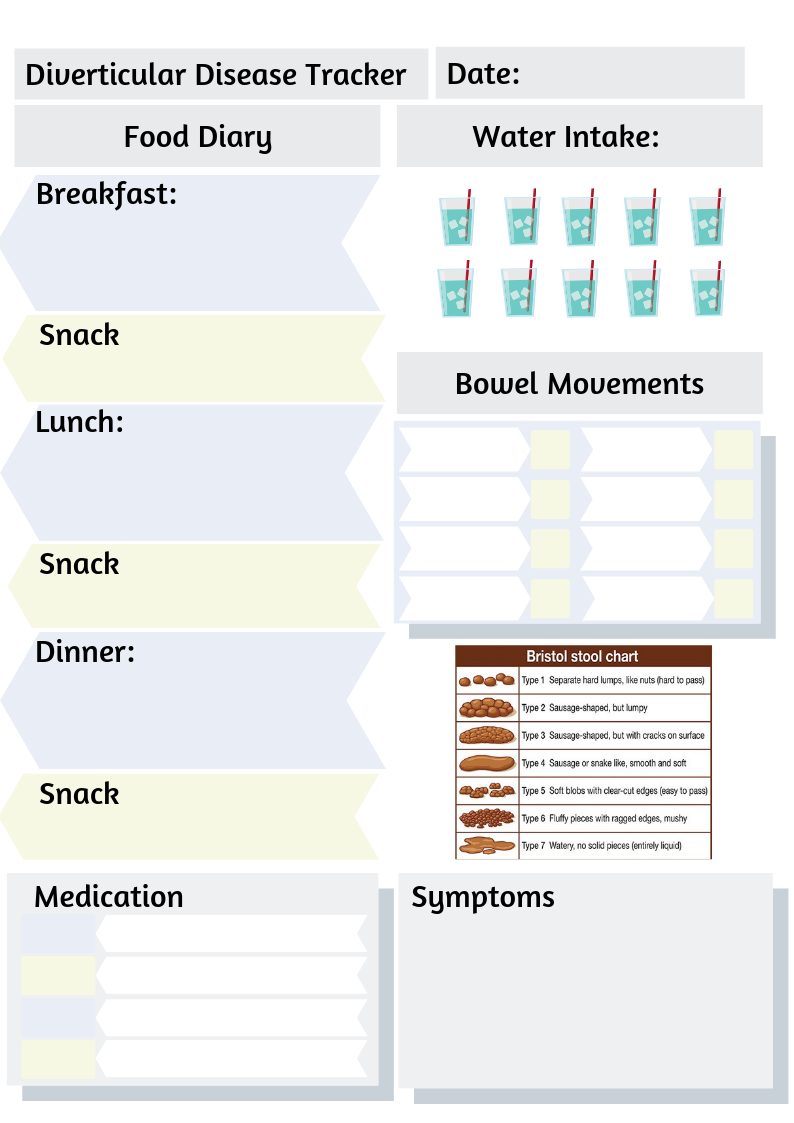
A lot of discovering what you can eat, is about trial and error. Everyone is different. Many people with diverticular disease/diverticulosis also suffer with other digestive problems such as IBS that can cause symptoms in response to particular foods. So my advice is that if you are feeling unwell, you can try an elimination diet, or you can simply go day by day and keep track of your food intake by keeping a food diary. I’d recommend for those newly diagnosed especially, keeping track of your food and water intake, your symptoms and your bowel movements. You can do this easily using the Diverticular Disease/Diverticulosis Tracker which you can find here and download for free. It includes instructions for how to fill it out. You can even take your completed tracker pages to the doctor or nutritionist so that they can help you look at what foods may or may not work well with you and your needs.

Some advice I can give to ALL sufferers of Diverticular Disease/Divertiulosis is to drink LOTS of water. Two to three litres (4 – 6 pints/70-100 fl. oz) per day. This will help keep you hydrated, healthy and prevent constipation. Also chew your food well and avoid large portions. In fact, simply following my Tips for Good Digestion may help you avoid digestive discomfort.